Measuring Local-Area Racial Segregation for Medicare Hospital Admissions
JAMA Network Open
Ellesse-Roselee L. Akré, Deanna Chyn, Heather A. Carlos, Amber E. Barnato, Jonathan Skinner
Considerable racial segregation exists in U.S. hospitals which cannot be explained by where patients live. Using 2019 Medicare claims data linked to geographic data, we define a hospital’s market based on ZIP-code based driving time, and estimate the racial composition of all hospitalizations in that market. We then compare the racial composition of the hospital with the racial composition of its market. In our sample of 4.9 million hospital admissions, we find a considerable degree of sorting, with Black Medicare enrollees more likely admitted to some hospitals in their market, and less likely to be admitted to other hospitals nearby. At a regional level, we observed the greatest degree of patient sorting in the New York, Chicago, and Detroit HRRs.
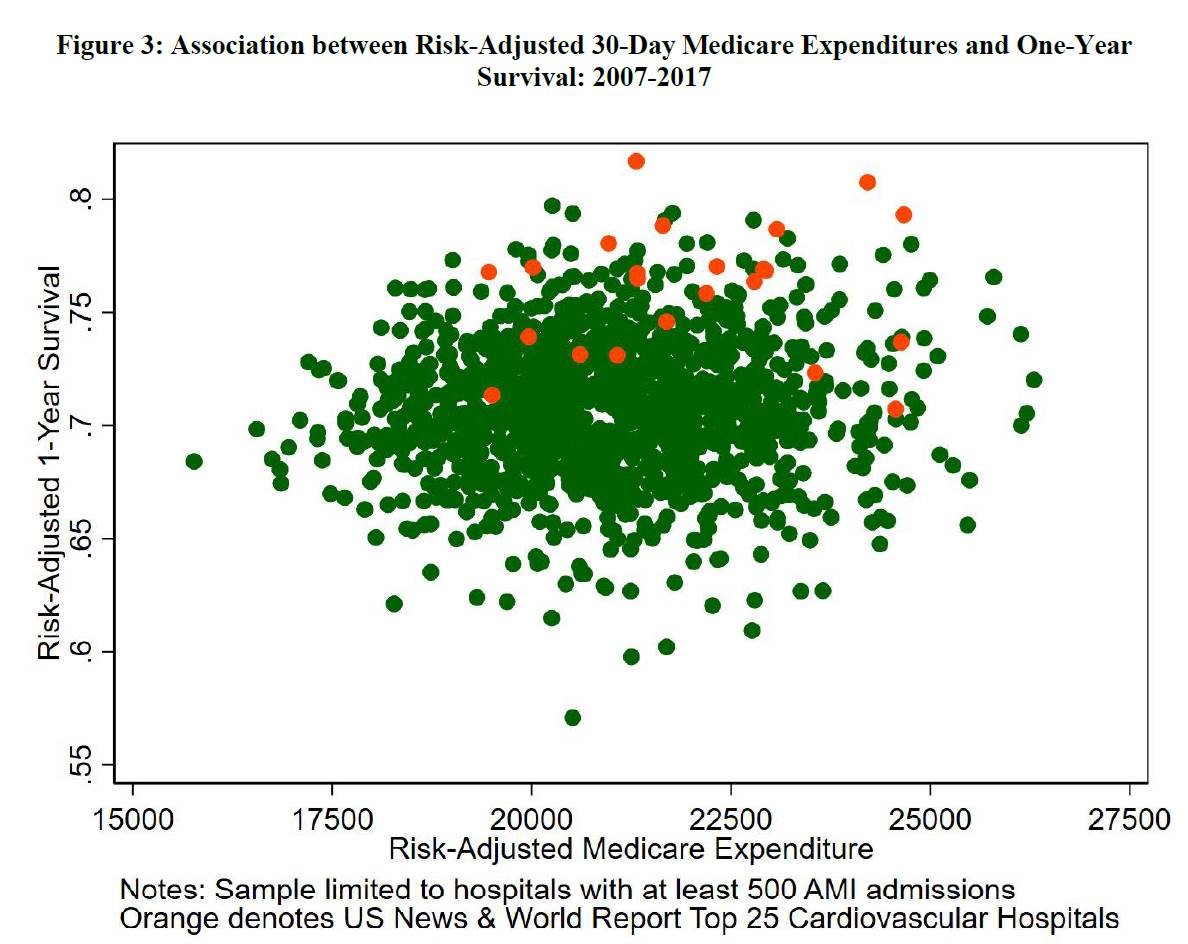
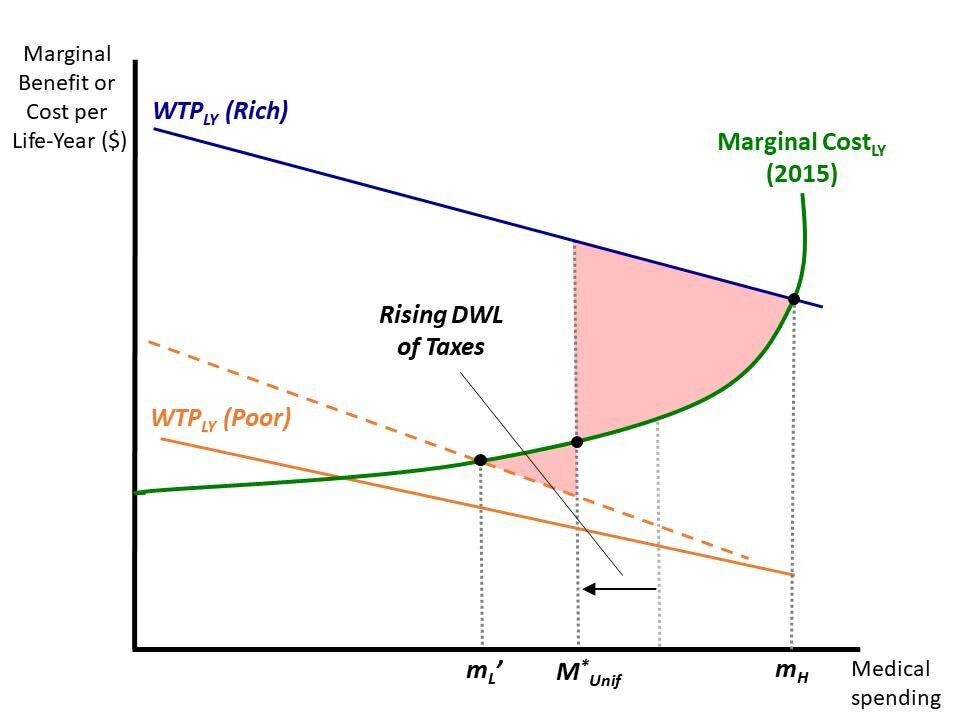
Productivity Variation and Input Misallocation: Evidence from Hospitals
NBER WORKING PAPER SERIES
Amitabh Chandra, Carrie H. Colla and Jonathan S. Skinner
There are widespread differences in total factor productivity across producers in the U.S. and around the world. To help explain these variations, we devise a general test for misallocation in input choices – the underuse of effective inputs and overuse of ineffective ones. Misallocation implies that conditional on total input use, the return to using a particular input is not zero (a positive return implies underuse, and a negative return implies overuse). We measure misallocation across hospitals, where inputs and outputs are better measured than in other industries. Applying our test to a sample of 1.6 million Medicare beneficiaries with heart attacks (of which 436 thousand were admitted by ambulance), we reject the hypothesis of productive efficiency; moving a patient from a 10th percentile to a 90th percentile hospital with respect to misallocation, holding spending constant, is predicted to increase survival by 3.1 percentage points. With misallocation accounting for as much as 25 percent of the variation in hospital productivity, our results suggest that how the money is spent, rather than how much money is spent, is central to understanding productivity differences both in health care, and in the rest of the economy.
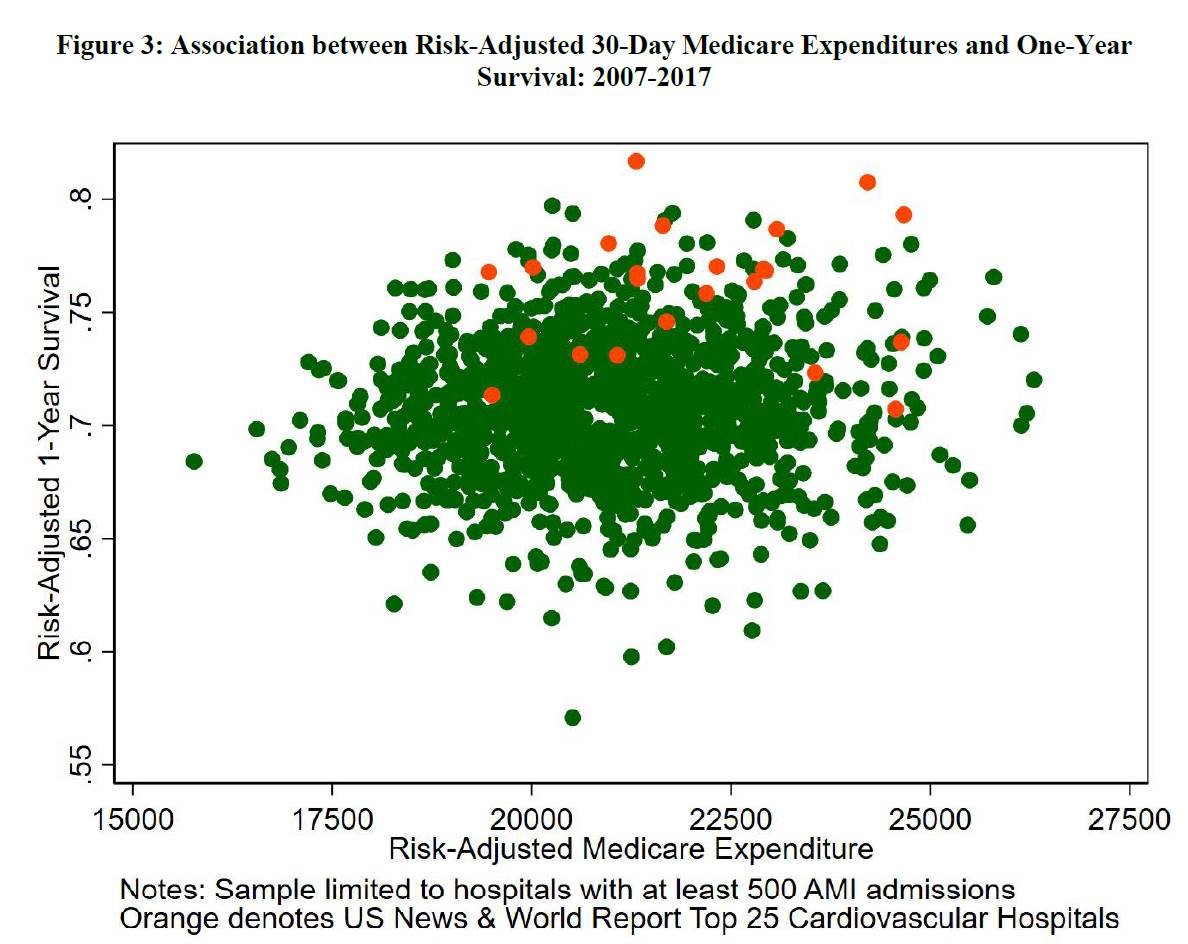
The diffusion of health care fraud: A bipartite network analysis
Social Science & Medicine
James O’Malley, Thomas Bubolz, Jonathan Skinner
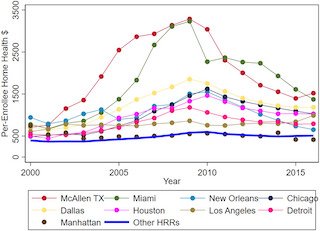
Many studies have examined the diffusion of health care innovation but less is known about the diffusion of health care fraud. In this paper, we consider the diffusion of potentially fraudulent Medicare home health care billing in the United States during 2002–16, with a focus on the 21 hospital referral regions (HRRs) covered by local Department of Justice (DOJ) anti-fraud “strike force” offices. We hypothesize that patient-sharing across home health care agencies (HHAs) provides a mechanism for the rapid diffusion of fraudulent strategies. We measure such activity using a novel bipartite mixture (or BMIX) network index, which captures patient sharing across multiple agencies and thus conveys more information about the diffusion process than conventional unipartite network measures. Using a complete population of fee-for-service Medicare claims data, we first find a remarkable increase in home health care activity between 2002 and 2009 in many regions targeted by the DOJ; average billing per Medicare enrollee in McAllen TX and Miami increased by $2127 and $2422 compared to just an average $289 increase in other HRRs not targeted by the DOJ…

Geographical Variation in Health Spending Across the US Among Privately Insured Individuals and Enrollees in Medicaid and Medicare
JAMA Network Open
Zack Cooper, Olivia Stiegman, Chima D. Ndumele, Becky Staiger, Jonathan Skinner
While the Dartmouth Atlas has established the wide variation in spending and utilization across the U.S. for older Medicare enrollees, much less is known about small-area variations for across all 3 major funders of health care in the US: Medicare, Medicaid, and private insurers.
This study first asks whether either spending or utilization (hospital days) are correlated across Medicare, Medicaid, and the privately insured, to see whether there are regions with simultaneously low spending across all payers, and to test which factors are associated with spending and utilization. The Figure above is the overall composite measure of health care spending in 2016-17 across 3 payers.
Listen to Podcast: Geographic Variations on a Healthcare Spending Theme 8/4/22
Read more and download the data here:

Rising Geographic Disparities in US Mortality
Journal of Economic Perspectives
Benjamin K. Couillard, Christopher L. Foote, Kavish Gandhi, Ellen Meara, and Jonathan Skinner
The 21st century has been a period of rising inequality in both income and health. In this paper, we find that geographic inequality in mortality for midlife Americans increased by about 70 percent between 1992 and 2016. This was not solely because of the increasing importance of “deaths of despair,” or by rising spatial income inequality during the same period. Instead, we find evidence that high-income states in 1992 were better able to enact public health strategies and adopt behaviors that, over the next quarter-century, resulted in pronounced relative declines in mortality. The substantial longevity gains in high-income states led to greater cross-state inequality in mortality.

THE DIFFUSION OF HEALTH CARE FRAUD: A NETWORK ANALYSIS
NBER Working Paper
A. James O’Malley, Thomas A. Bubolz, Jonathan S. Skinner
Many studies have examined the diffusion of health care innovations but less is known about the diffusion of health care fraud. In this paper, we consider the diffusion of potentially fraudulent Medicare home health care billing in the United States during 2002-16, with a focus on the 21 hospital referral regions (HRRs) covered by local Department of Justice anti-fraud “strike force” offices. We hypothesize that patient-sharing across home health care agencies provides a mechanism for the rapid diffusion of fraudulent strategies; we measure such activity using a novel bipartite mixture (or BMIX) network index. First, we find a remarkable increase in home health care activity between 2002 and 2009 in some but not all regions; average billing per Medicare enrollees in McAllen TX and Miami increased by $2,127 and $2,422 compared to a $289 increase in other HRRs not targeted by the Department of Justice. Second, we establish that the HRR-level BMIX (but not other network measures) was a strong predictor of above-average home care expenditures across HRRs. Third, within HRRs, agencies sharing more patients with other agencies were predicted to increase spending the following year. Finally, the initial 2002 BMIX index was a strong predictor of subsequent changes in HRR-level home health billing during 2002-9. These results highlight the importance of bipartite network structure in diffusion and in infection models more generally.

Comparing Health Outcomes of Privileged US Citizens With Those of Average Residents of Other Developed Countries
JAMA Internal Medicine
Ezekiel J. Emanuel, Emily Gudbranson, Jessica Van Parys, Mette Gørtz, Jon Helgeland, Jonathan Skinner
The average health outcomes in the US are not as good as the average health outcomes in other developed countries. However, whether high-income US citizens have better health outcomes than average individuals in other developed countries is unknown. OBJECTIVE To assess whether the health outcomes of White US citizens living in the 1% and 5%richest counties (hereafter referred to as privileged White US citizens) are better than the health outcomes of average residents in other developed countries.

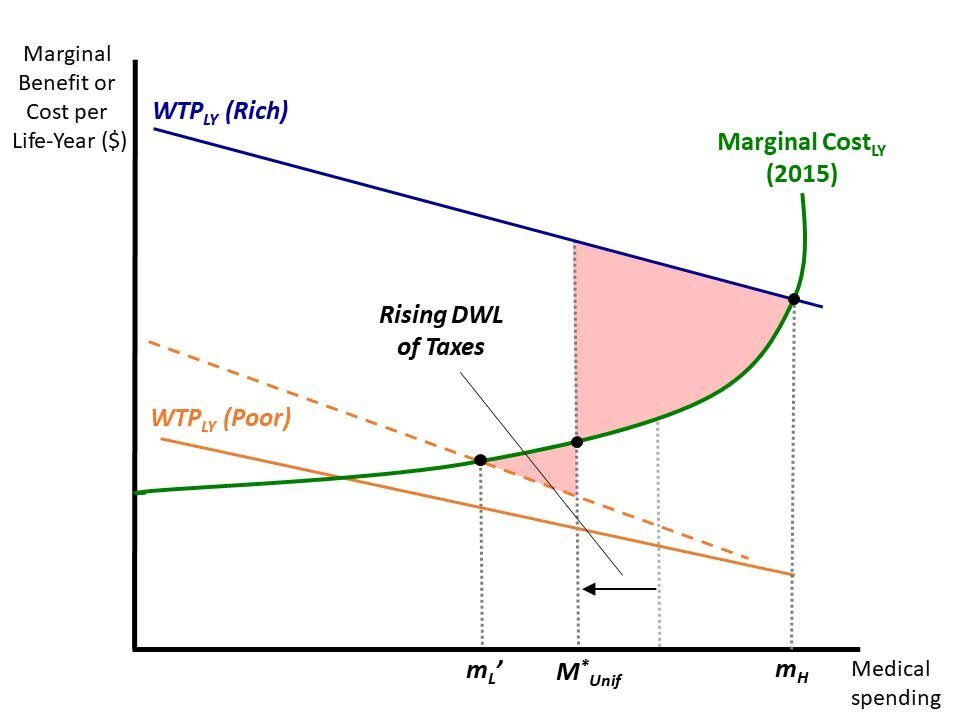
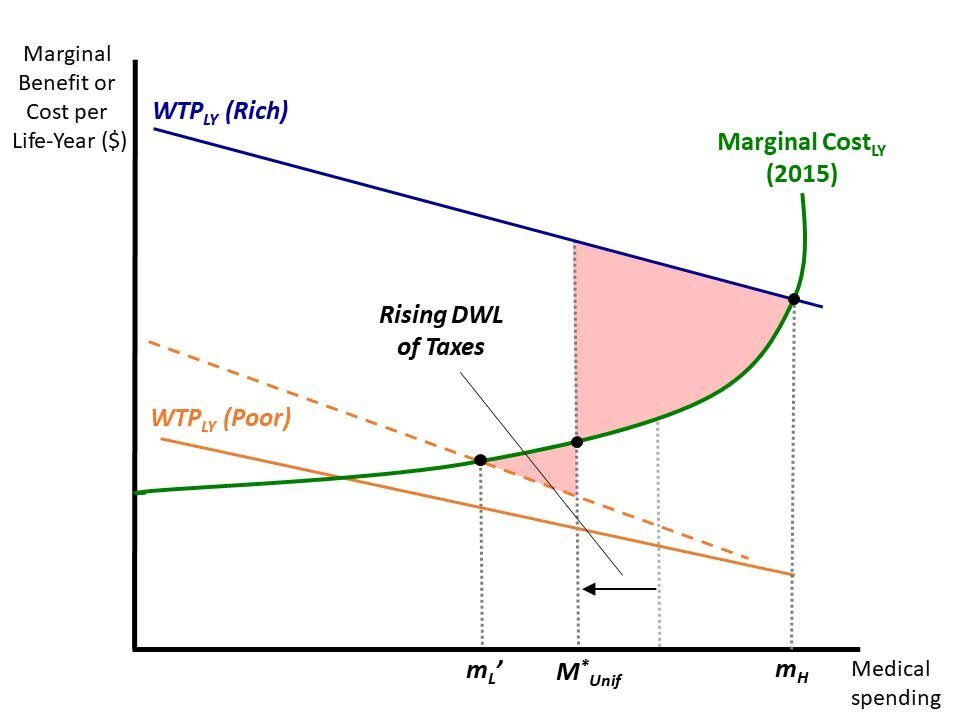
Does One Medicare Fit All? The Economics of Uniform Health Insurance Benefits
NBER Working Paper
Mark Shepard, Katherine Baicker and Jonathan S. Skinner
There is increasing interest in expanding Medicare health insurance coverage in the U.S., but it is not clear whether the current program is the right foundation on which to build. Traditional Medicare covers a uniformset of benefits for all income groups and provides more generous access to providers and new treatments than public programs in other developed countries. We develop an economic framework to assess the efficiency and equity tradeoffs involved with reforming this generous, uniform structure. We argue that three major shifts make a uniform design less efficient today than when Medicare began in 1965. First, rising income inequality makes it more difficult to design a single plan that serves the needs of both higher- and lower-income people. Second, the dramatic expansion of expensive medical technology means that a generous program increasingly crowds out other public programs valued by the poor and middle class. Finally, as medical spending rises, the tax-financing of the system creates mounting economic costs and increasingly untenable policy constraints. These forces motivate reforms that shift towards a more basic public benefit that individuals can “top-up” with private spending. If combined with an increase in other progressive transfers, such a reform could improve efficiency and reduce public spending while benefiting low income populations.

The Impact Of The COVID-19 Pandemic On Hospital Admissions In The United States
Health Affairs
John D. Birkmeyer, Amber Barnato, Nancy Birkmeyer, Robert Bessler, and Jonathan Skinner
Hospital admissions in the US fell dramatically with the onset of the coronavirus disease 2019 (COVID-19) pandemic. However, little is known about differences in admissions patterns among patient groups or the extent of the rebound. In this study of approximately 1 million medical admissions from a large nationally representative hospitalist group, we found that declines in non-COVID-19 admissions from February to April 2020 were generally similar across patient demographic subgroups and exceeded 20% for all primary admission diagnoses. By late June/early July 2020, overall non-COVID-19 admissions had rebounded to 16% below pre-pandemic baseline volume (8% including COVID-19 admissions). Non-COVID-19 admissions were substantially lower for patients residing in majority-Hispanic neighborhoods (32% below baseline) and remained well below baseline for patients with pneumonia (−44%), COPD/asthma (−40%), sepsis (−25%), urinary tract infection (−24%) and acute ST-elevation myocardial infarction (STEMI), −22%). Health system leaders and public health authorities should focus on efforts to ensure that patients with acute medical illnesses can obtain hospital care as needed during the pandemic to avoid adverse outcomes.

Residential Setting and the Cumulative Financial Burden of Dementia in the 7 Years Before Death
Journal of the American Geriatric Society
Kelley AS, McGarry K, Bollens-Lund E, Rahman OK, Husain M, Ferreira KB, Skinner JS.
Care for older adults with dementia during the final years of life is costly, and families shoulder much of this burden. We aimed to assess the financial burden of care for those with and without dementia, and to explore differences across residential settings. Using the Health and Retirement Study (HRS) and linked claims, we examined total healthcare spending and proportion by payer-Medicare, Medicaid, out-of-pocket, and calculated costs of informal caregiving-over the last 7 years of life, comparing those with and without dementia and stratifying by residential setting. We found that, consistent with prior studies, people with dementia experience significantly higher costs, with a disproportionate share falling on patients and families. This pattern is most striking among community residents with dementia, whose families shoulder 64% of total expenditures (including $176,180 informal caregiving costs and $55,550 out-of-pocket costs), compared with 43% for people with dementia residing in nursing homes ($60,320 informal caregiving costs and $105,590 out-of-pocket costs). These findings demonstrate disparities in financial burden shouldered by families of those with dementia, particularly among those residing in the community. They highlight the importance of considering the residential setting in research, programs, and policies.

Physician Beliefs and Patient Preferences: A New Look at Regional Variation in Health Care Spending
American Economic Journal
David Cutler, Jonathan S. Skinner, Ariel Dora Stern, and David Wennberg*
There is considerable controversy about the causes of regional variations in health care expenditures. Using vignettes from patient and physician surveys linked to fee-for-service Medicare expenditures, this study asks whether patient demand-side factors or physician supply-side factors explain these variations. The results indicate that patient demand is relatively unimportant in explaining variations. Physician organizational factors matter, but the most important factor is physician beliefs about treatment. In Medicare, we estimate that 35 percent of spending for end-of-life care and 12 percent of spending for heart attack patients (and for all enrollees) is associated with physician beliefs unsupported by clinical evidence. (JEL D83, H75, I11, I18)

Exnovation of Low Value Care: A Decade of Prostate-Specific Antigen Screening Practices
Journal of the American Geriatrics Society
Julie Bynum, MD, MPH,*†‡ Honor Passow, PhD,‡ Donald Carmichael, MDiv,‡ and Jonathan Skinner, PhD‡§¶
Using PSA screening, we aimed to understand which factors influence practice change during a period when a decline in service use would be expected. First, we focused on national PSA screening in men aged 68 and older with fee-for-service Medicare from 2003 to 2013 and examine the influence of guidelines by assessing changes in likelihood of screening associated with factors directly mentioned in guidelines. Second, we focused on practice change across U.S. hospital referral regions (HRRs) for men aged 75 and older – for whom guidelines have been in agreement – to test whether practice variation declines and what contextual factors are associated with greater decline. We hypothesized that guidelines and the practice environment would influence the degree to which practitioners and patients would reduce their use of an existing practice in the face of converging evidence regarding effectiveness.

Validating Publicly Available Crosswalks for Translating ICD-9 to ICD-10 Diagnosis Codes for Cardiovascular Outcomes Research
Cardiovascular Quality and Outcomes
Jesse A. Columbo, Ravinder Kang, Spencer W. Trooboff, Kristen S. Jahn, Camilo J. Martinez, Kayla O. Moore, Andrea M. Austin, Nancy E. Morden, Corinne G. Brooks, Jonathan S. Skinner, Philip P. Goodney
We devised an 8-step process to derive and validate ICD10 codes from an existing set of ICD-9 codes representing outcomes across several body systems (Figure 1). This process was developed in an iterative fashion with input from all coauthors and shared with collaborators as part of an ongoing National Institute on Aging Program Project (P01-AG019783).

Big Ideas in Health Economics
Health Affairs
Jonathan S. Skinner
Health economics as a profession has grown exponentially in the past half-century, but not everyone agrees on what health economics is. Many physicians think that health economists spend their days tabulating prices for cost-effectiveness studies. I once was called by a large pharmaceutical company seeking to recruit a health economist. Puzzled as to why any profitable company would want to employ me, I asked what they meant by “health economics.” With a sigh, the recruiter responded: “To prepare a business case for marketing new drugs.”

Mandatory Medicare Bundled Payment Program for Lower Extremity Joint Replacement and Discharge to Institutional Postacute Care: Interim Analysis of the First Year of a 5-Year Randomized Trial
JAMA
Amy Finkelstein, PhD; Yunan Ji, BA; Neale Mahoney, PhD; Jonathan Skinner, PhD
As part of a 5-year, mandatory-participation randomized trial by the Centers for Medicare & Medicaid Services, eligible metropolitan statistical areas (MSAs) were randomized to the Comprehensive Care for Joint Replacement (CJR) bundled payment model for LEJR episodes or to a control group. In the first performance year, hospitals received bonus payments if Medicare spending for LEJR episodes was below the target price and hospitals met quality standards. This interim analysis reports first-year data on LEJR episodes starting April 1, 2016, with data collection through December 31, 2016.

Health Care Employment Growth and the Future of US Cost Containment
JAMA
Jonathan Skinner, PhD; Amitabh Chandra, PhD
In 2013, the growth rate in US health care spending of 3.6% was the lowest in 50 years. Health policy experts and the media viewed the “unprecedented” decline as demonstrating that growth in health care costs had finally slowed.1 However, one number that was not consistent with this popular narrative was employment growth in the health care sector. In 2013, health care jobs continued to increase by 1.4%, slightly below the annual average of 1.9% during the prior 5 years.
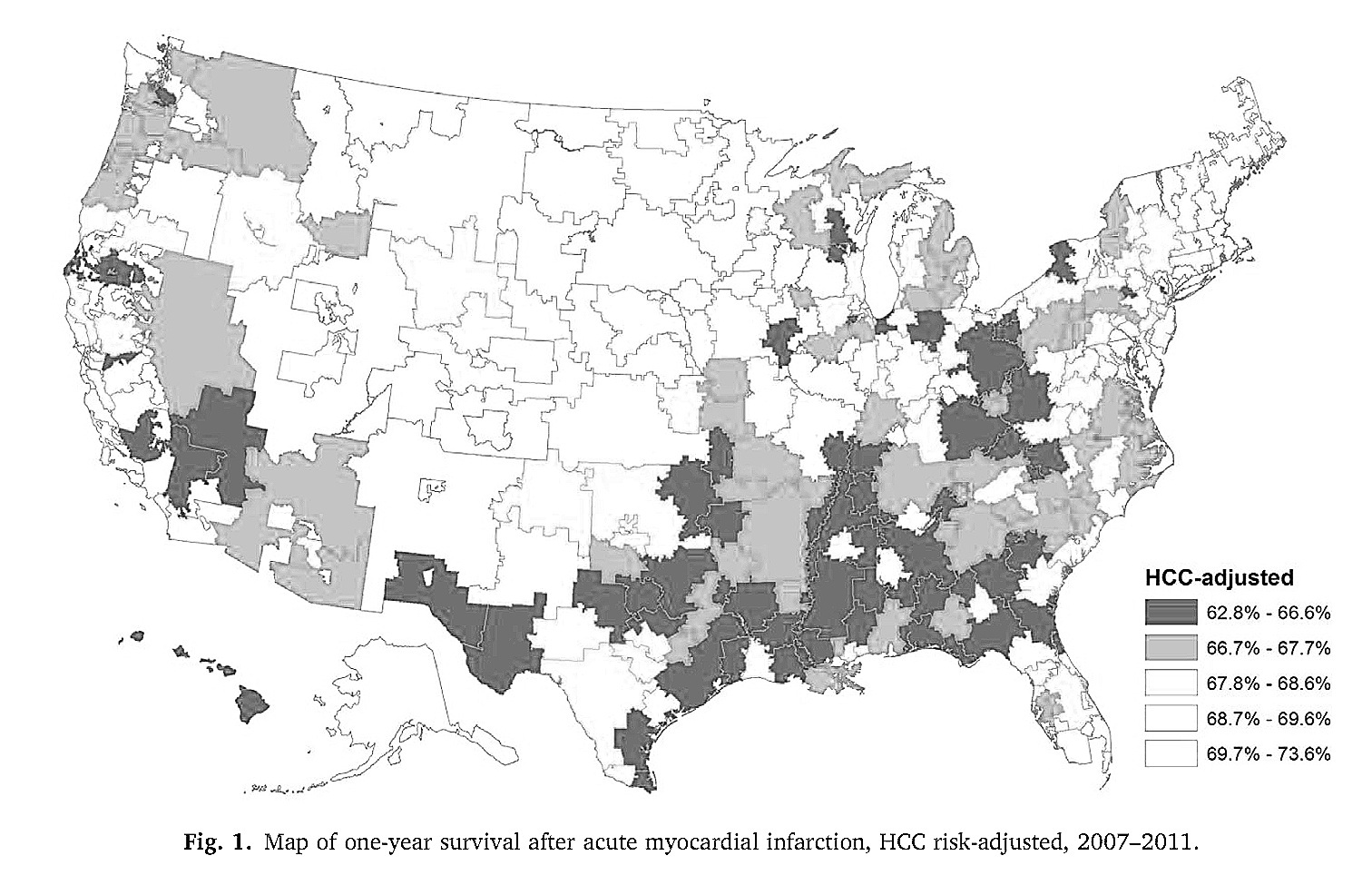
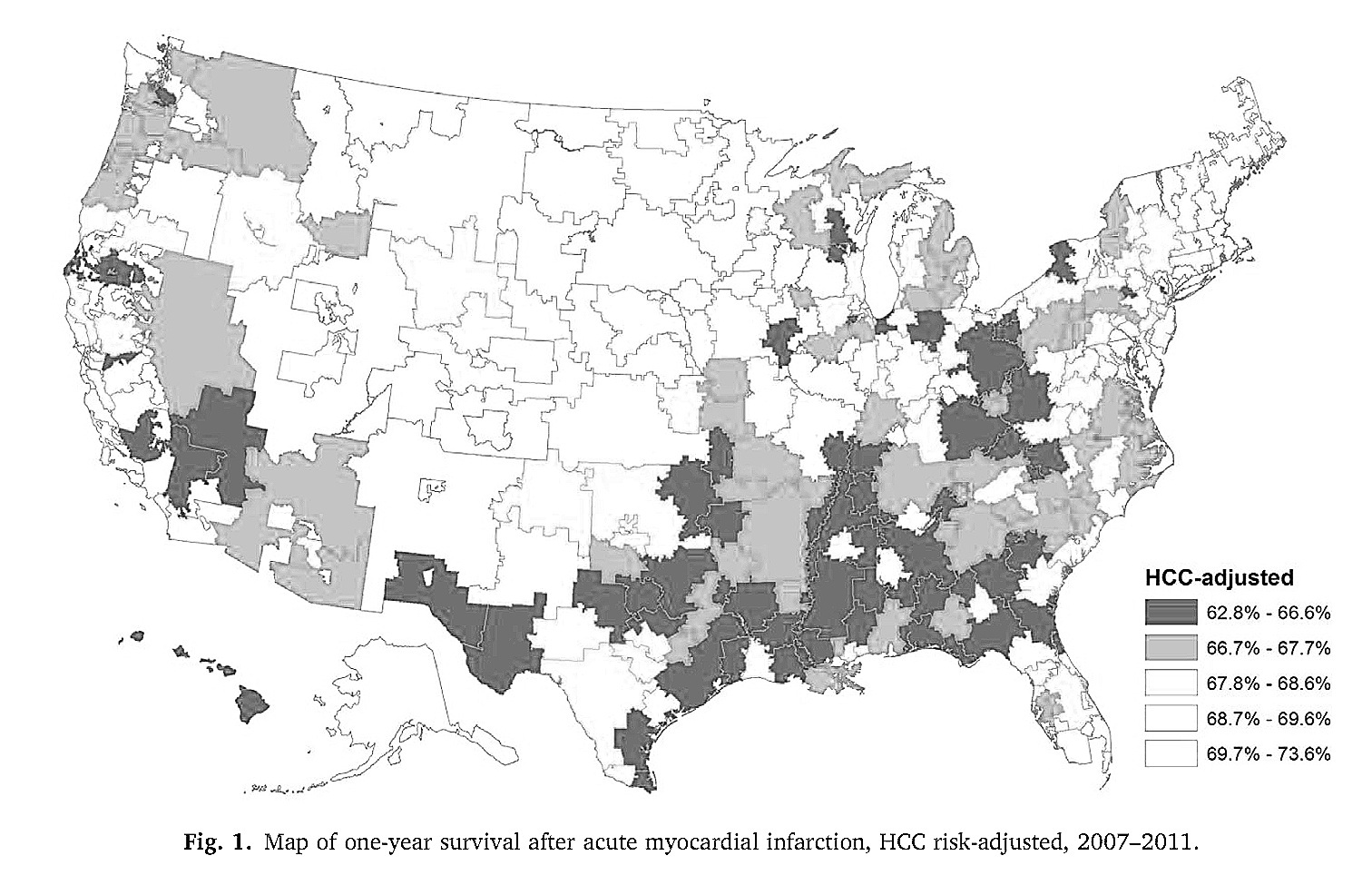
The association between medical care utilization and health outcomes: A spatial analysis
Regional Science & Urban Economics
Francesco Moscone, Jonathan Skinner, Elisa Tosetti, Laura Yasaitis
As health care spending continues to strain government and household budgets, there is increasing interest in measuring whether the incremental dollar spent on health care is worth it. In studying this question, researchers often make two key assumptions: that health care intensity can be summarized by a single index such as average spending, and that samples of hospitals or regions are spatially independent: Manhattan and the Bronx are no more alike than are Manhattan and San Diego, for example. In this paper we relax both assumptions. Using detailed data on 897,008 elderly Medicare enrolees with acute myocardial infarction (or a heart attack) during 2007–11, we find first that the total level of health care spending has little impact on health outcomes; more important is how the money is spent. …